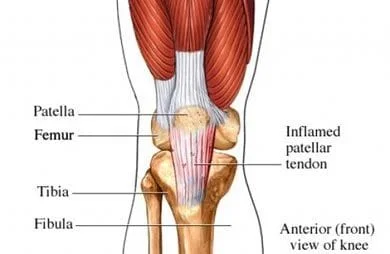
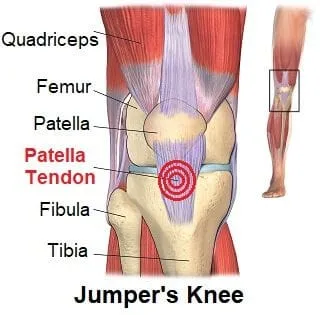
Patellar tendonitis, or more properly called patellar tendinopathy, and also called quadriceps tendonopathy or tendonitis, is the term for micro-tearing or degeneration of the patellar tendon, which is just below the knee cap.
Is this the same condition as "jumper's knee?"
The condition has been named “jumper’s knee” since excessive loading of the knee during high frequency repetitive jumping is considered the primary risk factor. The condition may more aptly named “landing knee” because research has shown forces placed on the tendon during landing are approximately double those created during the lift off phase (2,3,4). Activities that involve rapid acceleration and deceleration are also thought to place the patellar tendon at risk (5).
How common is patellar tendonitis?
Patellar tendinopathy is common, affecting up to 20% of athletes with a prevalence as high as 50% in sports which require repetitive forceful jumping and landing like volleyball and basketball (6,7). Interestingly, when the condition is present only on one side, it affects males more commonly at a ratio of 2:1. When the problem presents on both sides, both sexes are equally affected (6). Athletes who land with excessive foot inversion or allow deeper angles of knee flexion have a higher risk of developing the condition (7,8,9).
What are the symptoms of patellar tendonitis?
Symptoms are often chronic without an identifiable onset, sometimes relapsing or remitting over months or years. Symptoms are provoked by activity, but most athletes have been able to continue playing through the pain. Patients will report that pain intensifies when rising from a seated position, squatting, jumping, stair climbing or running- especially downhill or downstairs (10).
Two-thirds of patients present with pain in the characteristic inferior patellar location.
Do patellar tendonitis patients have tight or weak quadriceps?
Patients with patellar tendinopathy often demonstrate quadriceps and hamstring tightness with associated myofascial involvement. Additionally, quadriceps weakness is common in patellar tendonitis patients. Compensatory mechanisms to protect the knee may result in secondary problems throughout the lower kinetic chain.
Are x-rays or imaging necessary?
Imaging may be unnecessary unless a history of trauma, surgery, or joint swelling in older individuals. MRI to diagnose patellar tendinopathy is questionable (14, 15).
What is the best treatment for patellar tendonitis?
The foundation for clinical management of patellar tendonitis includes anti-inflammatory modalities, transverse friction massage, and eccentric exercise. Modalities including ultrasound, interferential, and ice may help diminish inflammation.
Some athletes may need to decrease training amount and intensity to reduce the load to a sub-pain threshold level.
Stretching and myofascial release techniques should be directed at areas of concern in the hamstring, quadriceps, and calves. Additional areas of myofascial concern would include the iliotibial band, psoas, piriformis and anterior hip capsule. Transverse friction massage or IASTM is thought to improve clinical outcomes by stimulating a healing response (18).
Manipulation may be necessary for restrictions in the ankle, knee, hip or lumbosacral region.
Do I need to rest with patellar tendonitis?
Patellar tendonitis patients should avoid complete rest, as this could actually increase the risk of recurrence (17). Ice or ice massage should be used at home and after activity.
What does rehab look like for patellar tendonitis?
Rehabilitation of patellar tendonitis typically progresses from selective rest to functional re-training. The goal of tendinopathy rehab is to carefully balance a controlled inflammatory response without causing greater injury or exacerbating symptoms. Rehab should begin with moderate effort and low repetitions. Response to rehab may be assessed by the patient’s change in night pain. Increases in night pain indicate the current rehab load is excessive. Progression advances when the patient tolerates a given level of load. (29)
Eccentric exercise along with static stretching is a vastly superior mode of treatment for patellar tendonitis (19,20,21).
What about a patellar tendon strap?
Patellar tendon straps, like a DonJoy Cross Strap, ProTec or Cho-Pat, are thought to slightly reorient the patellar tendon, thereby reducing stress on the most vulnerable fibers (27). The majority of people utilizing patellar tendon straps report improvement (23)
What about other treatments?
In general, patients undergoing surgery for patellar tendinopathy show similar outcomes to those undergoing eccentric strengthening program (24). Stubborn cases may consider PRP or steroid injections.
At Creekside Chiropractic & Performance Center, we are highly trained to treat patellar tendonitis. We are the only inter-disciplinary clinic providing services to Sheboygan, Sheboygan Falls, Plymouth, and Oostburg including chiropractic, manual therapy, myofascial release, ART (Active Release Technique), massage therapy, acupuncture, physiotherapy, rehabilitative exercise, nutritional counseling, personal training, and golf performance training under one roof. Utilizing these different services, we can help patients and clients reach the best outcomes and the best versions of themselves. Voted Best Chiropractor in Sheboygan by the Sheboygan Press.
Evidence Based-Patient Centered-Outcome Focused
Sources:
1. Johnson DP, Wakeley CJ, Watt I. Magnetic resonance imaging of patellar tendonitis. J Bone Joint Surg Br. 1996;78:452–7
2. Brukner, P. and K.M. Khan, Chapter 2: Sports Injuries, in Clinical Sports Medicine, P. Brukner and K.M. Khan, Editors. 1993, McGraw-Hill: Sydney.
3. Garrick, J.G. and D.R. Webb, Sports Injuries: Diagnosis and management. 1990, Philadelphia: Saunders. xi, 347.
4. Richards, D.P., et al., Knee joint dynamics predict patellar tendinitis in elite volleyball players. American Journal of Sports Medicine, 1996. 24(5): p. 676-683.
5. . Fredberg, U. and L. Bolvig, Jumper's knee. Review of the literature. Scandinavian Journal of Medicine and Science in Sports, 1999. 9(2): p. 66- 73.
6. Witvrouw E, Bellemans J, Lysens R, Danneels L, Cambier D. Intrinsic risk factors for the development of patellar tendinitis in an athletic population. A two-year prospective study. Am J Sports Med. Mar-Apr 2001;29(2):190-5
7. Lian OB, Engebrestsen L, Bahr R. Prevalence of jumper’s knee among elite athletes from different sports. Am J Sports Med. 2005;33:561–7
8. Lian Ø, Engebretsen L, Ovrebø RV, Bahr R. Characteristics of the leg extensors in male volleyball players with jumper’s knee. Am J Sports Med. 1996;24:380-385.
9. Lian Ø, Refsnes PE, Engebretsen L, Bahr R. Performance characteristics of volleyball players with patellar tendinopathy. Am J Sports Med. 2003;31:408-413.
10. Visentini PJ, Khan KM, Cook JL, Kiss ZS, Har- court PR, Wark JD. The VISA score: an index of severity of symptoms in patients with jumper’s knee (patellar tendinosis). Victorian Institute of Sport Tendon Study Group. J Sci Med Sport. 1998;1:22-28.
11. Khan KM, Maffulli N, Coleman BD, Cook JL, Taunton JE. Patellar tendinopathy: some aspects of basic science and clinical management. Br J Sports Med. 1998;32:346–55
12. Leonardo Addêo Ramos et al. Prevalence of Pain on Palpation of the Inferior Pole of the Patella Among Patients with Complaints of knee Pain Clinics. 2009 March; 64(3): 199–202
13. Almekinders LC, Vellema JH, Weinhold PS. Strain patterns in the patellar tendon and the implications for patellar tendinopathy. Knee Surg Sports Traumatol Arthrosc. 2002;10:2-5.
14. Dixit S, Difor JP., Management of Patellofemoral Pain Syndrome. Am Fam Physician. 2007 Jan 15;75(2):194-202.
15. Shalaby M, Almekinders LC. Patellar tendinitis: the significance of magnetic resonance imaging findings. Am J Sports Med. 1999;27:345–9
16. Brukner P, Khan K, McConnell J, Cook J. Anterior knee pain. In: Brukner P, Khan K. Clinical Sports Medicine. 2nd ed. New York, N.Y.: McGraw- Hill, 2002:464–93.
17. Rutland M, O’Connell D, Evidence Supported Rehabilitation of Patellar Tendonorathy, N Am J of Sports PT, 2010 September; 5(3): 168-178
18. Wilson JK, Sevier TL, Helfst R, et al. Comparison of rehabilitation methods in the treatment of patellar tendinitis. Journal of Sports Rehabilitation2000;9:304–14.
19. Dimitrios S, Pantelis M, Kalliopi S, Comparing the effects of eccentric training with eccentric training and static stretching exercises in the treatment of patellar tendinopathy. A controlled clinical trial. Clin Rehabil. 2012 May;26(5):423-30.
20. Purdam CR, Jonsson P, Alfredson H, et al. A pilot study of the eccentric decline squat in the management of painful chronic patellar tendinopathy. British Journal of Sports Medicine. 2004 Aug;38(4):395-7.
21. Larsson ME, Käll I, Nilsson-Helander K. Treatment of patellar tendinopathy -- a systematic review of randomized controlled trials. Knee Surgery, Sports Traumatology, Arthroscopy. 2011 Dec 21
22. Stasinopoulos D and Stasinopoulos I. Comparison of effects of exercise programme, pulsed ultrasound and transverse friction in the treatment of chronic patellar tendinopathy. Clin Rehabil 2004; 18: 347–352
23. Michael Lavagnino, PhD, et al. Infrapatellar Straps Decrease Patellar Tendon Strain as the Site of the Jumper's Knee Lesion: A Computational Analysis Based on Radiographic Measurements. In Sports Health. May/June 2011. Vol. 3. No. 3. Pp. 296-302
24. Bahr R, Fossan B, Løken S, et al. Surgical treatment compared with eccentric training for patellar tendinopathy (Jumper's Knee). A randomized, controlled trial. Journal of Bone and Joint Surgery. American volume. 2006 Aug;88(8):1689-98.
25. Ferretti, A., P. Papandrea, and F. Conteduca, Knee injuries in volleyball. Sports Medicine, 1990. 10(2): p. 132-138.
26. Dedes V, Stergioulas A, Kipreos G, Dede AM, Mitseas A, Panoutsopoulos GI. Effectiveness and Safety of Shockwave Therapy in Tendinopathies. Mater Sociomed. 2018 Jun;30(2):131-146. doi: 10.5455/msm.2018.30.141-146.
27. Sprouse RA et al. Braces and Splints for Common Musculoskeletal Conditions. Am Fam Physician. 2018 Nov 15;98(10):570-576.
28. Rio E, Kidgell D, Purdam C, et al. Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy. Br J Sports Med. 2015;49:1277-1283.
29. Cook JL, Purdam CR. The challenge of managing tendinopathy in competing athletes. Br J Sports Med. 2014;48:506-509.