MCL and LCL: Medial Collateral Ligament and Lateral Collateral Ligament
Knee stability is derived primarily from the four major ligaments: the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), medial collateral ligament (MCL), and lateral collateral ligament (LCL).
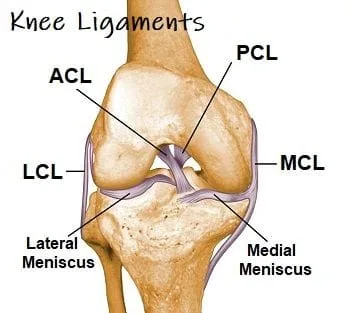
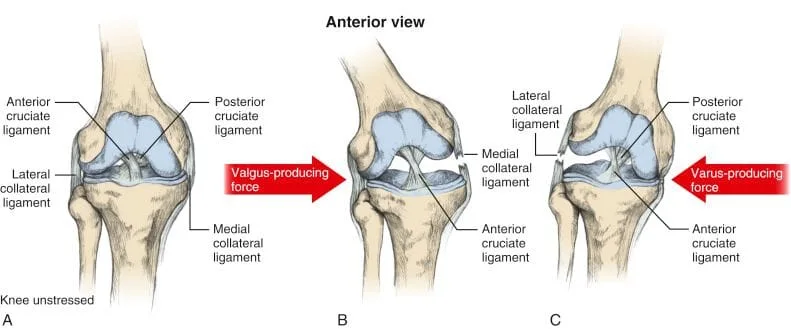
The Medial Collateral Ligament originates from the medial (inside) aspect of the femur and inserts onto the tibia (shinbone). The lateral collateral ligament (LCL), sometimes called the “fibular collateral ligament”, originates on the lateral aspect of the femur and inserts \on the fibular head (2,5). These ligaments are in charge of limiting valgus and varus motion in the knee.
Which is more common to injure, MCL or LCL?
The MCL is the most commonly injured ligament of the knee (6-8) and accounts for almost 8% of all athletic injuries. (9) The primary mechanism for MCL injury involves application of a sudden outside to inside (valgus) stress such as a direct hit to the lateral knee, while the foot is planted (10). The incidence of MCL injury is higher in football, skiing, ice hockey, wrestling, rugby, and judo (8,11-14).
The LCL is the least commonly injured ligament of the knee (15). The typical mechanism of LCL injury involves the opposite of what caused the MCL injury, which would be an inside to outside stress, which is usually combined with hyperextension of the knee (16).
How are knee ligament injuries graded?
Ligament injuries are traditionally classified as Grade I, Grade II, or Grade III
Grade I- stretch with no visible fiber disruption
Grade II- partial fiber disruption
Grade III-Rupture
Unfortunately, significant knee trauma is capable of producing a multi-ligament injury. In fact, a Grade III MCL sprain results in associated ACL disruption in more than 75% of cases (20,21). A combined injury of the MCL, ACL and meniscus is termed an “unhappy triad” or “blown knee”.
What are the symptoms of a collateral ligament sprain?
The typical symptoms of collateral ligament sprain includes pain on the inside or outside aspect of the knee following trauma, i.e. sporting event or vehicular accident (15). Patients will often report hearing a “pop” with pain following. Decreased range of motion is common and attributed to pain and swelling. Increases in activity usually make the pain worse. Trouble walking is possible and not unusual. Some patients feel "weak" or unstable. Clicking is possible, and is generally seem with damage to the meniscus as well.
Do I need X-rays for a MCL or LCL sprain?
The Ottowa knee rule suggests that X-rays be performed in any patient with acute knee injury plus any of the following criteria: age over 55, isolated tenderness of the knee cap or fibular head, inability to flex the knee beyond 90 degrees, inability to bear weight for four steps (31,32).
Advanced imaging of knee sprains is generally unnecessary- as skilled clinical evaluation may detect knee injury with similar sensitivity to MRI (50). Advanced imaging should be reserved for pre-operative planning or investigating suspicions of multiple injuries (mensical tear, etc.) (35,50).
What are the best treatment options for MCL or LCL sprains?
The management of collateral ligament sprains has shifted to a more conservative, non-surgical approach (27,39-46). The rehabilitation of collateral ligament sprain can be divided into three phases.
Phase I of Rehab
The Phase I of treatment seeks to promote optimal conditions for healing- keeping torn fibers close together as well as controlling and limiting motion (especially valgus, varus, or rotational movements that place extra stress on the structures) (45).
Grade II injuries require a hinged brace, and Grade III sprains recommend 1-6 weeks of immobilization to maintain a stable environment for healing. (39,40) . Depending upon the severity of tear, crutches may be necessary until the patient is able to walk normally (40). To encourage cartilage nourishment, it is suggested that those with injuries get rid of crutches as soon as they are able (39).
Like most other types of sprains, the early management of collateral ligament injury involves a RICES protocol: rest, ice, compression, elevation and support (23,40). Controlled early motion may help accelerate collagen synthesis (39). Range of motion exercises should begin in a gentle non-painful pendulum of flexion- extension (39).
How do I know that I have completed Phase I of rehab?
The patient has completed Phase I rehab when they are able to attain full weight bearing with normal gait (39).
Phase II of Rehab
The goal of Phase II includes restoring a full, pain-free range of motion while increasing strength. Research has shown that closed chain kinetic exercises are most appropriate (39,40,47). Early aerobic activity could include a stationary bicycle, elliptical stepper, or water aerobics.
Myofascial release and stretching may be appropriate for the surrounding musculature. The use of IASTM may be appropriate and accelerate healing for Grade I or II ligament sprains (48).
When can I progress to Phase III?
The Final phase of rehabilitation can begin when there is full range of motion with no significant swelling (39).
Phase III of Rehab
The goal of Phase III is to return to functional activity through endurance exercise, proprioceptive training, and functional/agility drills. Straight-line running is allowed when the patient is able to bear weight comfortably. A running program begins with jogging and progresses into sprinting, then narrow S-shaped patterns, and finally sports specific agility drills.
When can I return to activity after an LCL or MCL sprain?
Return to full activity is dependent upon the degree of injury, as well as the location of tear, any other injuries, age, and activity demands (39). Most Grade I and II injuries can return to play within 1-3 weeks, while Grade III injuries require 6 weeks or more to heal (40). A hinged knee brace may be necessary to protect the knee from repeat injury during activity.
What are other treatment options?
Surgery is reserved for knees that are functionally unstable or for patients with persistent pain and/or disability, despite conservative treatments (16,23).
At Creekside Chiropractic & Performance Center, we are highly trained to treat MCL and LCL sprains. We are the only inter-disciplinary clinic providing services to Sheboygan, Sheboygan Falls, Plymouth, and Oostburg including chiropractic, manual therapy, myofascial release, ART (Active Release Technique), massage therapy, acupuncture, physiotherapy, rehabilitative exercise, nutritional counseling, personal training, and golf performance training under one roof. Utilizing these different services, we can help patients and clients reach the best outcomes and the best versions of themselves. Voted Best Chiropractor in Sheboygan by the Sheboygan Press.
Evidence Based-Patient Centered-Outcome Focused
Sources:
1. LaPrade RF, Engebretsen AH, Ly TV, Johansen S, Wentorf FA, Engebretsen L. The anatomy of the medial part of the knee. J Bone Joint Surg Am. 2007;89:2000–2010.
2. Wheeless Textbook of Orthopedics. Medial Collateral ligament. Duke Orthopaedics. www.wheelessonline.com\ortho\medial_collateral_ligament. Accessed 11/20/14.)
3. Phisitkul P, James SL, Wolf BR, Amendola A. MCL injuries of the knee: current concepts review. Iowa Orthop J. 2006;26:77–90.
4. Grood ES, Noyes FR, Butler DL, Suntay WJ. Ligamentous and capsular restraints preventing straight medial and lateral laxity in intact human cadaver knees. J Bone Joint Surg Am. 1981;63:1257–1269.
5. Meister BR, Michael SP, Moyer RA, Kelly JD, Schneck CD. Anatomy and kinematics of the lateral collateral ligament of the knee. Am J Sports Med. 2000;28:869–878.
6. S.L. Woo, M. Inoue, E. McGurk-Burleson, et al. Treatment of the medial collateral ligament injury II: structure and function of canine knees in response to differing treatment regimens Am J Sports Med, 15 (1) (1987), pp. 22–29
7. Agranoff AB et al. Medial Collateral and Lateral Collateral Ligament Injury. http://emedicine.medscape.com/article/307959-overview. accessed 11/26/14
8. Roach CJ, Haley CA, Cameron KL, Pallis M, Svoboda SJ, Owens BD. The epidemiology of medial collateral ligament sprains in young athletes. Am J Sports Med. May 2014;42(5):1103-9.
9. Schulz MS, Russe K, Weiler A, Eichhorn HJ, Strobel MJ. Epidemiology of posterior cruciate ligament injuries. Arch Orthop Trauma Surg. 2003;123:186–191.
10. Indelicato PA. Isolated medial collateral ligament injuries in the knee. J Am Acad Orthop Surg. 1995;3:9–14.
11. Bradley J, Honkamp NJ, Jost P, West R, Norwig J, Kaplan LD. Incidence and variance of knee injuries in elite college football players. Am J Orthop (Belle Mead NJ) 2008;37:310–314.
12. Warme WJ, Feagin JA, Jr, King P, Lambert KL, Cunningham RR. Ski injury statistics, 1982 to 1993, Jackson Hole Ski Resort. Am J Sports Med. 1995;23:597–600.
13. Flik K, Lyman S, Marx RG. American collegiate men’s ice hockey: an analysis of injuries. Am J Sports Med. 2005;33:183–187.
14. Levy AS, Wetzler MJ, Lewars M, Laughlin W. Knee injuries in women collegiate rugby players. Am J Sports Med. 1997;25:360–362.
15. Logerstedt DS, Snyder-Mackler L, Ritter RC, Axe MJ, Godges JJ. Knee Stability and Movement Coordination Impairments: Knee Ligament Sprain J Orthop Sports Phys Ther. Apr 2010; 40(4): A1–A37.
16. DeCarlo M, Armstrong B. Rehabilitation of the Knee Following Sports Injury. Clinics in Sports Medicine. Volume 29, Issue 1, Pages 81–106, January 2010
17. A. Tria, K. Klein An illustrated guide to the knee Churchill Livingstone, New York (1991)
18. LaPrade RF, Gilbert TJ, Bollom TS, Wentorf F, Chaljub G. The magnetic resonance imaging appearance of individual structures of the posterolateral knee. A prospective study of normal knees and knees with surgically verified grade III injuries. Am J Sports Med. 2000;28:191–199.
19. LaPrade RF, Terry GC. Injuries to the posterolateral aspect of the knee. Association of anatomic injury patterns with clinical instability. Am J Sports Med. 1997;25:433–438
20. Halinen J, Lindahl J, Hirvensalo E, Santavirta S. Operative and nonoperative treatments of medial collateral ligament rupture with early anterior cruciate ligament reconstruction: a prospective randomized study. Am J Sports Med. 2006;34:1134–1140.
21. Fetto JF, Marshall JL. Medial collateral ligament injuries of the knee: a rationale for treatment. Clin Orthop Relat Res. 1978:206–218.
22. Brukner P, Khan K. Clinical Sports Medicine.
23. Sydney, Australia: McGraw-Hill Australia; 2006.
24. Y. Tegner, J. Lysholm Rating systems in the evaluation of knee ligament injuries Clin Orthop Relat Res, 198 (1985), pp. 43–49
25. Waldman SD. Chapter 149 – Medial Collateral Ligament Tear. 2011, Imaging of Pain Pages 381–383
26. D. Daniel, M. Stone Diagnosis of keen ligament injury: tests and measurements of joint laxity J.A. Feagin (Ed.), The Crucial Ligaments (1st Edition), Churchill Livingstone, New York (1988), pp. 287–300
27. Phisitkul P, James SL, Wolf BR, Amendola A. MCL injuries of the knee: current concepts review. Iowa Orthop J. 2006;26:77–90.
28. Bates, Barbara. 1974. A Guide to Physical Examination. J.B. Lippincott Company, Toronto.
29. Kastelein M, Wagemakers HP, Luijsterburg PA, Verhaar JA, Koes BW, Bierma-Zeinstra SM. Assessing medial collateral ligament knee lesions in general practice. Am J Med. 2008;121:982–988. e982.
30. Reider B. Medial collateral ligament injuries in athletes. Sports Med. 1996;21:147–156.
31. Bachmann LM, Haberzeth S, Steurer J, ter Riet G. The accuracy of the Ottawa knee rule to rule out knee fractures: a systematic review. Ann Intern Med. 2004;140:121–124.
32. Stiell IG, Greenberg GH, Wells GA, et al. Derivation of a decision rule for the use of radiography in acute knee injuries. Ann Emerg Med. 1995;26:405–413.
33. Goela, Amini B. et. al. Pellegrini-stieda lesion radiopaedia.org. Obtained from Radiopaedia.org\articles\pellegrini-stieda-lesion on 11/20/14)
34. Kocabey Y, Tetik O, Isbell WM, Atay OA, Johnson DL. The value of clinical examination versus magnetic resonance imaging in the diagnosis of meniscal tears and anterior cruciate ligament rupture. Arthroscopy. 2004;20:696–700.
35. Chahal J, Al-Taki M, Pearce D, et al. Injury patterns to the posteromedial corner of the knee in high-grade multiligament knee injuries: a MRI study. Knee Surg Sports Traumatol Arthrosc. Dec 15 2009
36. Robertson A, Nutton RW, Keating JF. Dislocation of the knee. J Bone Joint Surg Br. 2006;88:706–711.
37. Bachmann LM Robertson A, Nutton RW, Keating JF. Dislocation of the knee. J Bone Joint Surg Br. 2006;88:706–711.,
38. Haberzeth S, Steurer J, ter Riet G. The accuracy of the Ottawa knee rule to rule out knee fractures: a systematic review. Ann Intern Med. 2004;140:121–124.
39. DeCarlo M, Armstrong B. Rehabilitation of the Knee Following Sports Injury. Clinics in Sports Medicine. Volume 29, Issue 1, Pages 81–106, January 2010
40. DeBerardino TM. Medial Collateral Knee Ligament Injury Treatment & Management Medscape. Accessed 9/12/14. http://emedicine.medscape.com/...
41. K.D. Shelbourne, D.V. Patel Management of combined injuries of the anterior cruciate and medial collateral ligaments Instr Course Lect (1996), pp. 45275–45280
42. D.E. Hastings The non-operative management of collateral ligament injuries of the knee joint Clin Orthop Relat Res (1980), pp. 14722–14728
43. R. Sandberg, B. Balkfors, B. Nilsson, et al. Operative versus non-operative treatment of recent injuries to the ligaments of the knee. A prospective randomized study J Bone Joint Surg, 69 (8) (1987), pp. 1120–1126
44. K.D. Shelbourne, J.R. Baele Treatment of combined injuries of the anterior cruciate and medial collateral ligaments J Bone Joint Surg (1988), pp. 156–158
45. K.E. Wilk, J.R. Andrews, W.G. Clancy Nonoperative and postoperative rehabilitation of the collateral ligaments of the knee Oper Tech Sports Med (1996), pp. 4192–4201
46. Indelicato PA, Hermansdorfer J, Huegel M. Nonoperative management of complete tears of the medial collateral ligament of the knee in intercollegiate football players. Clin Orthop Relat Res. 1990:174–177.
47. R.A. Palmitier, K.-N. An, S.G. Scott, et al. Kinetic chain exercise in knee rehabilitation Sports Medicine, 11 (1991), p. 402
48. Loghmani MT, Stuart Warden Instrument-Assisted Cross-Fiber Massage Accelerates Knee Ligament Healing Orthop Sports Phys Ther 2009;39(7):506-514.
49. Laprade RF, Bernhardson AS, Griffith CJ, Macalena JA, Wijdicks CA. Correlation of valgus stress radiographs with medial knee ligament injuries: an in vitro biomechanical study. Am J Sports Med. Feb 2010;38(2):330-8.
50. Kocabey Y, Tetik O, Isbell WM, Atay OA, Johnson DL. The value of clinical examination versus magnetic resonance imaging in the diagnosis of meniscal tears and anterior cruciate ligament rupture. Arthroscopy. 2004;20:696–700.
51. Laprade RF, Bernhardson AS, Griffith CJ, et al. Correlation of valgus stress radiographs with medial knee ligament injuries: an in vitro biomechanical study. Am J Sports Med. Dec 4 2009.

