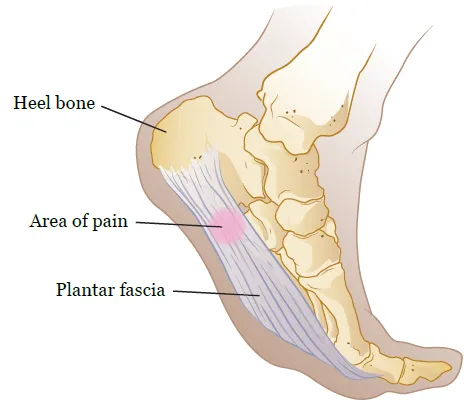
The plantar fascia is a dense, fibrous band that sttabilizes and protects structures on the plantar (bottom) aspect of the foot. The diagnosis “plantar fasciitis” includes acute inflammation and pain to chronic degeneration (1,2). Plantar fasciitis most commonly affects the middle portion of the band (2).
What is the most common cause of heel pain?
Plantar fasciitis is the most common cause of plantar heel pain, affecting about 10 percent of the population (14-18).
Can I have plantar fasciitis in both feet?
The condition is seen in both feet in 20-30 percent of patients (19).
Who is most likely to get plantar fasciitis?
It is quite common in young runners and middle-aged women, but most plantar fascia patients are over the age of 40 (16-18).
What causes plantar fasciitis?
The cause of plantar fasciitis is multi-factorial, many of which are biomechanical changes in the foot (21). Fallen arches (flat feet) are the top cause. Those with excessively high arches are also vulnerable (22). Tightness or weakness in the calf muscles also contribute to plantar fasciitis by increasing strain on the plantar fascia (25-27). Patients with plantar fasciitis are almost 9 times more likely to demonstrate hamstring tightness, which places an increased strain on the fascia as well (29,30). Weight gain and obesity are also recognized contributors to plantar fasciitis (17,25).
What activities or jobs can cause plantar fasciitis?
Jobs or recreational activities that include prolonged standing including: teachers, construction workers, cooks, nurses, distance runners, etc.
How much pressure does the plantar fascia have to absorb with each step?
The plantar fascia must absorb up to seven times (7x) body weight during the push off phase of running
What are the symptoms of plantar fasciitis?
The most common complaint of plantar fasciitis is a sharp pain with the first few steps in the morning or any period of inactivity (16,25). Symptoms are often noted during the push off phase of the step (32). Symptoms are amplified by prolonged standing, especially when compounded by inadequate foot support or walking barefoot (25). Walking up stairs, sprinting, or forefoot running tends to worsen symptoms by increasing plantar fascia strain. Patients report relief when unloading the foot by sitting or lying down.
Do I need x-rays or imaging for plantar fasciitis?
Radiographs are typically not required for the diagnosis of plantar fasciitis (51). Radiographs may, however, be useful in differentiating plantar fasciitis if other diagnoses are suspected, such as a stress fracture.
What about heel spurs?
X-rays commonly show heel spurs. Numerous studies demonstrate no correlation between spur size and the patient’s subjective complaints (52). Heel spurs are considered coincidental and irrelevant findings (53). They are an after effect rather than a cause of the process (54,55).
What causes a heel spur?
Spurs are thought to develop when long-standing tension creates stress where the fascia attaches to the bone. The presence of a heel spur suggests abnormal stress in the region for at least six months (56). Heel spurs are present in approximately 50% of patients with foot pain and 15-20 percent of patients without pain (54,57).
Do I need treatment for heel spurs?
As stated before, heel spurs are usually the effect of some other process and are not typically the source of a patient's pain. Getting treatment in the area including manual therapy, adjustments of the foot bones, exercises to strengthen/stretch the foot musculature, and other therapies may be beneficial, but the heel spur will most likely remain (and that's okay).
How long do plantar fasciitis symptoms last?
While a treatment plan may last a few weeks to get pain and function under control, plantar fasciitis is somewhat of a nagging-type injury. Almost half of plantar fasciitis sufferers will continue to report pain 10 years after onset (101).
What are the best treatments for plantar fasciitis?
Conservative treatment, including manual therapy, stretching, myofascial release, exercise, orthotics, physical therapy modalities, and night splints may improve results (61-63). The best treatment outcomes are achieved by combining multiple techniques- particularly mobilization and exercise (63,97).
What activity modifications do I need to do for plantar fasciitis?
Patients may need to temporarily limit activities that worsen symptoms, including jumping, running, and sprinting. Once patients find a tolerable level of activity, they should not increase their training intensity by more than 10% per week (64).
Running with plantar fasciitis
Runners should avoid running hills, and toe or forefoot runners may need to temporarily alter their running form. Runners may benefit by reducing stride length and increasing cadence (36). Running shoes lose half of their shock absorption capacity after 300-500 miles and should be replaced within that range (65,88,89). Safer alternatives include swimming, biking, and elliptical machines (66).
Do I need orthotics for plantar fasciitis?
Patients who hyperpronate and those with fallen arches will benefit from arch supports or orthotics (67). Patients may also benefit from a heel cup or small cushion donut on the heel (70). The use of kinesiology tape (Rocktape, etc.) has been proposed for the treatment of plantar fasciitis.
Do I need a boot or a night splint for plantar fasciitis?
Immobilizing tissue in a stretched state speeds recovery (71). Chronic plantar fasciitis patients may benefit from using a boot or night splint (Strassburg sock), which allows the plantar fascia to “heal” in a lengthened or stretched state (92,93).
What are the best shoes for plantar fasciitis?
Patients with low arches may benefit from “motion control” shoes (such as shoes for overpronators). Runners with neutral arches should choose “neutral” or “stability” shoes (72). Patients with high arches may benefit from a “cushioned” shoe (73).
Are NSAIDs such as tylenol, ibuprofen, or aleve helpful?
Since most chronic cases of plantar fasciits do not show histologic evidence of inflammation, the benefit of “anti-inflammatory” modalities is questionable (74). Some patients report at least palliative relief by using NSAIDs, ice, and modalities.
Can Creekside help plantar fasciitis?
In short, yes. Our treatments may include ankle joint mobilization and manipulation to help restore normal necessary motion (76,77,90). The addition of calf and plantar fascia trigger point work including Active Release Technique produces superior short-term outcomes (62). Myofascial release procedures, including transverse friction massage and IASTM (Graston, etc.) are effective tools that may stimulate fibroblast proliferation and plantar fascia regeneration (79,80,95).
Can I do things at home to help plantar fasciitis?
We suggest stretching exercises to the gastroc, soleus, hamstring, and plantar fascia (81,91). Routinely stretching the plantar fascia in this fashion is associated with significantly improved outcomes (81). Plantar fascia mobilization may be performed at home by rolling a golf ball or frozen water bottle beneath the plantar fascia.
Strengthening exercises can also be implemented for the gastroc, soleus, posterior tibialis, and intrinsic muscles of the foot (82). Examples include marble and towel gripping exercises. Strengthening exercises for the posterior tibialis muscle should be implemented to assist in arch support.
Do I need surgery for plantar fasciitis?
Nearly two-thirds of foot and ankle orthopedic specialists prefer stretching and manual therapy (conservative treatment) over anti-inflammatories, steroid injections, or surgery for chronic plantar fasciitis patients (83). Cases that are unresponsive typically involve a fasciotomy surgery to release the plantar fascia.
At Creekside Chiropractic & Performance Center, we are highly trained to treat plantar fasciitis. We are the only inter-disciplinary clinic in Sheboygan county that provides chiropractic, myofascial release, ART (Active Release Technique), massage therapy, acupuncture, physiotherapy, rehabilitative exercise, nutritional counseling, personal training, and golf performance training under one roof. Utilizing these different services, we can help patients and clients reach the best outcomes and the best versions of themselves. Voted Best Chiropractor by the Sheboygan Press.
Evidence Based-Patient Centered-Outcome Focused
Sources:
1. Kendrick Alan Whitney Plantar Fasciosis Copyright 2010-2013 Merck Sharp & Dohme Corp accessed 4/16/14
2. Thomas Michaud, Differential Diagnosis of Heel Pain Dynamic Chiropractic – January 15, 2013, Vol. 31, Issue 02
3. Michaud T. Foot Orthoses and Other Forms of Conservative Foot Care. 1st ed. Newton, MA: Thomas C Michaud; 1997.
4. Martin J, Hosch J, Goforth WP, Murff R, Lynch DM, Odom R. Mechanical Treatment of Plantar Fasciitis. Journal of the American Podiatric Association 2001; 91(2):55-62.
5. Aldridge T. Diagnosing Heel Pain in Adults. American Family Physician 2004; 70(2):332-8.
6. Fillipou D, Kalliakmanis A, Triga A, Rizos A, Grigoriadis E. Sport Related Plantar Fasciitis. Current Diagnostic and Therapeutic Advances. Folia Medica 2004; 46(3):56-60.
7. Wearing S, Smeathers J, Yates B, Sullivan P, Urry S, Dubois P. Sagittal Movement of the Medial Longitudinal Arch is Unchanged in Plantar Fasciitis. Medicine & Science in Sports & Exercise 2004; 36(10):1761-67.
8. Lemont H, Ammirati K, Usen N. Plantar Fasciitis:A Degenerative Process Without Inflammation. Journal of the American Podiatric Association 2003; 93(3):234-37.
9. Huang YC, Wang LY, Wang HC, Chang KL, Leong CP. The Relationship Between the Flexible Flatfoot and Plantar Fasciitis:Ultrasonographic Evaluation. Chang Gung Medical Journal 2004; 27(6):443-8.
10. Dyck D, Boyajian-O’Neill L. Plantar Fasciitis. Clinical Journal of Sports Medicine 2004; 14(5):305-309.
11. Cole C, Seto C, Gazewood J. Plantar Fasciitis: Evidence-Based Review of Diagnosis and Therapy. American Family Physician 2005; 72(11):2237-42.
12. Roxas M. Plantar Fasciitis:diagnosis and therapeutic considerations. Alternative Medicine Review 2005; 10(2):83-93.
14. DeMaio M, Paine R, Mangine RE, Drez DJr. Plantar fasciitis. Orthopedics 1993; 16:1153-1163.
15. Neufeld SK. Plantar Fasciitis: Evaluation and Treatment J Am Acad Orthop Surg June 2008 vol. 16 no. 6 338-346
16. Singh D, Angel J, Bentley G, Trevino SG. Fortnightly review. plantar fasciitis. BMJ. 1997;315:172-175.
17. DeMaio M, Paine R, Mangine RE, Drez D,Jr. Plantar fasciitis. Orthopedics. 1993;16:1153-1163.
18. Barrett SJ, O'Malley R. Plantar fasciitis and other causes of heel pain. Am Fam Physician. 1999;59:2200-2206.
19. Charles LM. Plantar fasciitis. Lippincotts Prim Care Pract. 1999;3:404-407
21. Gross MT, Byers JM, Krafft JL, Lackey EJ, Melton KM. The impact of custom semirigid foot orthotics on pain and disability for individuals with plantar fasciitis. J Orthop Sports Phys Ther. 2002;32:149-157.
22. Abreu M, Chung C, Mendes L, et al. Plan¬tar calcaneal enthesophytes: new obser-vations regarding sites of origin based on radiographic, MR imaging, anatomic, and paleopathologic analysis. Skeletal Radiol. 2003;32:13-21.
25. Young CC, Rutherford DS, Niedfeldt MW. Treatment of plantar fasciitis. Am Fam Physician. 2001;63:467-74, 477-8.
26. Schepsis AA, Leach RE, Gorzyca J. Plantar fasciitis. etiology, treatment, surgical results, and review of the literature. Clin Orthop. 1991; (266):185-196.
27. Bolivar YA, Munuera PV, Padillo JP. Relationship between tightness of the posterior muscles of the lower limb and plantar fasciitis. Foot Ankle Int. Jan 2013;34(1):42-8.
28. Bedi HS, Love BR. Differences in impulse distribution in patients with plantar fasciitis. Foot Ankle Int. 1998;19:153-156.
29. Labovitz JM, Yu J, Kim C. The role of hamstring tightness in plantar fasciitis. Foot Ankle Spec. 2011 Jun;4(3):141-4.
30. (Harty J, Soffe K, O’Toole G, and Stevens NM. The role of hamstring tightness in plantar fasciitis. Foot, ankle, int. 2005, December; 26 (12): 1089-92)
32. Michaud T, New Techniques For Treating Plantar Fasciitis Competitor Group Published Mar. 6, 2014
33. Boberg J, Dauphinee D. Plantar Heel. In: Banks AM, Downey D, Martin S, Miller. McGlamry's Comprehensive Textbook of Foot and Ankle Surgery. 1. 3. Philadelphia: Lippincott Williams & Wilkins; 2001:471.
34. DeGarceau D, Dean D, Requejo SM, Thordarson DB. The association between plantar fasciitis and Windlass test results. Foot & Ankle International 2004; 25(9):687-8
35. De Garceau D, Dean D, Requejo SM, Thordarson DB. The association between diagnosis of plantar fasciitis and Windlass test results. Foot Ankle Int. Mar 2003;24(3):251-5.
36. Michaud T, New Techniques For Treating Plantar Fasciitis Competitor Group Published Mar. 6, 2014
37. Wearing S, Smeathers J, Yates B, et al. Sagittal movement of the medial longitudi¬nal arch is unchanged in plantar fasciitis. Med Sci Sports Exerc. 2004;36:1761- 1767.
38. Menz H, Zammit G, Munteanu S, Scott G. Plantarflexion strength of the toes: age and gender differences and evaluation of a clinical screening test. Foot Ankle Int. 2006; 27:1103-1108.
39. Dirim B, Resnick D, Ozenler, N.K. Bilateral Baxter’s Neuropathy secondary to plantar fasciitis, Med Sci Monitor, 2010 April; 16 (4): CS 50-53.)
40. Delfaut EM, Demondion X, Bieganski A, Thiron MC, Mestdagh H, Cotten A. Imaging of foot and ankle nerve entrapment syndromes: from well- demonstrated to unfamiliar sites. Radiographics. 2003; 23:613-623.
41. Oztuna V, Ozge A, Eskandari MM, Colak M, Golpinar A, Kuyurtar F. Nerve entrapment in painful heel syndrome. Foot Ankle Int 2002; 23: 208- 211.
42. Chundru U, Liebeskind A, Seidelmann F, Fogel J, Franklin P, Beltran J. Plantar fasciitis and calcaneal spur formation are associated with abductor digiti minimi atrophy on MRI of the foot. Skeletal Radiol. 2008; 37:505-10.
43. Donovan A, Rosenberg ZS, Cavalcanti CF. MR imaging of entrapment neuropathies of the lower extremity. Part 2. The knee, leg, ankle, and foot. Radiographics. 2010; 30:1001-1019.
45. Baxter DE. Release of the nerve to the abductor digiti minimi. In: Kitaoka HB, ed. Master techniques in orthopaedic surgery of the foot and ankle. Philadelphia, PA: Lippincott Williams and Wilkins; 2002: 359.
46. Lui, TH. Endoscopic decompression of the first branch of the lateral plantar nerve. Arch Orthop Trauma Surg 2007; 127:859-61.